I worked in intensive care medicine for around five years. During this training I was fascinated by sepsis syndrome, or what is now called “Systemic Inflammatory Response Syndrome” or SIRS.
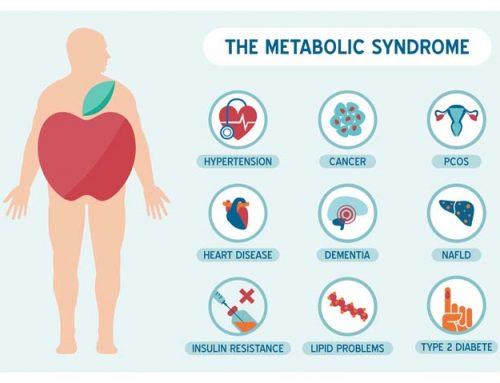
This syndrome often started with a fairly mild bacterial infection which spread to the bloodstream, and triggered a cascasde of events, often causing very low blood pressure, which would require intravenous fluids, antibiotics and even special medications inotropes to raise the blood pressure.
Initially research focused on the initial infection and treating that, however later experience and research really showed that even when the bacterial infection had been treated, there was an inflammatory cascade that was doing most of the damage. It was literally like a fire consuming everything up that came in its way.
Sometimes patients had to be ventilated due to a condition called ARDS where the patient’s lungs filled up with water. Sometimes they needed dialysis due to kidney failure due to poor blood flow. The heart could be affected too at times.
Research found that there are a number of inflammatory markers which are elevated in this syndrome, such as C4a, C5a, TGF-beta and MMP-9. Over in the distant waters of Pokomoke, Maryland, USA, a GP called Ritchie Shoemaker started asking similar questions about why people were getting unwell through contact with the waters of the Chesapake Bay, where fish were dying at the rate of knots.
After a dramatic recovery with a patient prescribed the bile acid binding resin cholestyramine for secretory diarrhoea, the first semblances of a theory came into place. Was some kind of toxin triggering a chain reaction of events, similar to in sepsis, but in a more chronic fashion? Could cholestyramine be binding these toxins and thereby lessening this inflammatory cascade?
Later came alligator kills due to blue-green algae in waterways in Florida. Then patients who were unwell due to exposure to water-damaged buildings. Mould wasn’t supposed to make you sick!
He started testing the same inflammatory markers that the ICU guys checked in patients with sepsis. Most of them were elevated in these folk. Sometimes C4a was in the tens of thousands, which means a major complement cascade was taking place. Due to mould? Surely not…
So if there was a reliable mechanism causing this inflammatory cascade, surely that would mean that a reliable treatment protocol could be created. Hence the birth of the Shoemaker protocol. More importantly it could provide hope to those who had been diagnosed with a disorder such a Chronic Fatigue Syndrome, fibromyalgia and other disorders with no clear biomarkers for diagnosis. And a clear path to recovery.
In the late 2000s a nasal spray of vasoactive intestinal polypeptide (VIP) seemed to be a major breakthrough in lowering cytokine levels, particularly C4a, MMP-9 and TGF-beta-1.
The research has continued to the stage where we have around 20 peer reviewed papers, on what has now being called chronic inflammatory response syndrome (CIRS). And although the research is ongoing, the question needs to be asked with all chronically ill patients with multisystem disorders, “is your patient suffering with a chronic version of sepsis syndrome?”
References:
- Shoemaker, R.C. & House, D.E. (2005). A time-series study of sick building syndrome: chronic, biotoxin-associated illness from exposure to water-damaged buildings. Neurotoxicology and teratology, 27(1), 29-46. PMID 15681119, Full text
- Shoemaker, R.C. (2001). Residential and recreational acquisition of possible estuary-associated syndrome: a new approach to successful diagnosis and treatment. Environmental health perspectives, 109 (suppl. 5), 791-6. PMID PMC1240613, Full text






Leave A Comment